Rectal Prolapse
Rectal prolapse is when part of the rectum protrudes from the anus. The rectum is the last part of the large intestine and is where feces is stored before being passed.
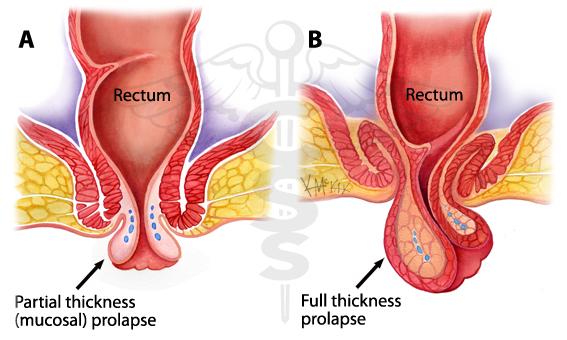
Prolapse occurs when the rectum becomes unattached inside the body and comes out through the anus, effectively turning itself inside out.
Rectal prolapse is a relatively rare condition, with the American Society of Colon and Rectal Surgeons estimating that it affects less than 3 in every 100,000 people.
Causes of Rectal Prolapse
There is a range of risk factors and causes associated with rectal prolapse, although doctors do not fully understand why some people get it.
It can be triggered by a variety of things including:
Pregnancy
Constipation or chronic straining
Diarrhea — present in around 15 percent of people
Conditions that make a person cough a lot
There are also some neurological conditions that affect the nerves associated with rectal prolapse:
Multiple sclerosis
Lumbar disc disease
Spinal tumors
Injury to the lower back or pelvis
Symptoms of Rectal Prolapse
At first, the person might only notice a lump or swelling coming out of their anus when they have a bowel movement.
Initially, the person may be able to push the rectal prolapse back in. Over time, however, the prolapse is likely to protrude permanently, and a person will be unable to push the prolapse back.
As time goes on, a rectal prolapse may happen when a person coughs, sneezes, or stands up. Some people with a rectal prolapse have described it as like "sitting on a ball."
Some people may experience an internal rectal prolapse, which is different in that the prolapse will not protrude. However, the person may feel as if they have not passed everything during a bowel movement.
Other symptoms of a rectal prolapse include:
difficulty controlling bowel movements, which occurs in around 50 to 75 percent of cases
bright red blood coming out of the rectum
discomfort
constipation, present in about 25 to 50 percent of people who have a rectal prolapse
Diagnostics of Rectal Prolapse
Your doctor will have you describe your symptoms and ask about your medical history. They should also do a complete physical examination. During your exam, your doctor may ask you to squat and strain as though you were having a bowel movement. Your doctor will observe your rectum and may placed a gloved finger in your anus to check the health or strength of the anal sphincter and the rectum itself.
You may also be directed to have a colonoscopy to check for any polyps.
Treatment of Rectal Prolapse
In the first instance, it is important to treat constipation. This might be achieved by eating plenty of foods that are high in fiber, such as fruit, vegetables, and wholegrains.
Bulking laxatives, which help a person have a bowel movement without straining, may also be recommended, as well as drinking plenty of water.
If that does not work, then surgery may be advised. The type of surgery will depend on a number of factors:
Type of prolapse
the person's age
other medical problems
whether the person is constipated or not
There are two general types of surgery for rectal prolapse:
Abdominal: Entry through the belly through a cut or several cuts in the abdominal wall. Often used for full-thickness prolapse.
Perineal: Involves STARR Surgery in which cutting out the full thickness segment of the prolapsing rectum is done endoscopiically using a stapler device. Suitable for people who cannot have a general anesthetic.